N.C. Governor, Roy Cooper extended the executive order of stay-at-home to May 8. This comes despite the growing protests for lifting the stay at home order for the state of Georgia, Tennessee and South Carolina.
Source The News & Observer.
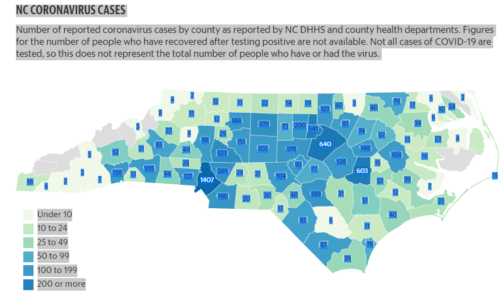
As of Friday, April 24, North Carolina has at least 7,821 reported cases of the coronavirus with 278 deaths, according to data collected by The News & Observer from state and county health departments. At least 486 North Carolinians are hospitalized with COVID-19 as of April 23 according to the N.C. Department of Health and Human Services.
Mecklenburg County has the highest numbers in the state with 1,377 reported cases and 37 deaths. Wake County has 633 cases and 11 deaths and Durham County has 500 cases and nine deaths. In the mountains, Buncombe County has 49 confirmed cases and three deaths, Henderson has 129 cases and 14 deaths, Macon county has two cases and one death, Haywood has five cases, and Jackson has three cases and no deaths.
Cooper’s decision is supported by states’ public health experts and is in line with what the medical community across the country including Anthony Fauchi and Dr. Sara Harkness.
“Continue to stay at home. This isn’t over yet. If we release the stay at home orders too early, expect to see a second wave of patients and more deaths,” warns Dr. Harkness, internal medicine physician in Oregon. WCJ reached to her for comment via instant message on Twitter.
Social distancing measurements were put in place to help lessen the spread of COVID-19 while also lessening the number of people needing inpatient hospital care. This would reduce the resources being utilized and beds being provided to COVID-19 patients.
Investigative reporting organization Propublica.org looked at hospitals and their capacities, and developed statistical scenarios to determine how the capacities of hospitals in U.S. will handle different percentages of the population infected with COVID-19. The data breaks down the rate of infection with social distancing measures over a period of 6 months, 12 months and 18 months. These scenarios are meant to show the overall benefit of social distancing can have on hospitals and lowering the demand.
“Hospitals in more urban communities will likely be more stressed, given the vast populations they serve,” is one of the conclusions of ProPublica.
In 2018, Asheville had 1,540 total hospital beds. In a moderate scenario with about 40% of Asheville’s population contracting the disease resulting in an influx of hospitalized patients that would require 1,590 beds over 12 months, which is 2.9 times the available beds in that time period.
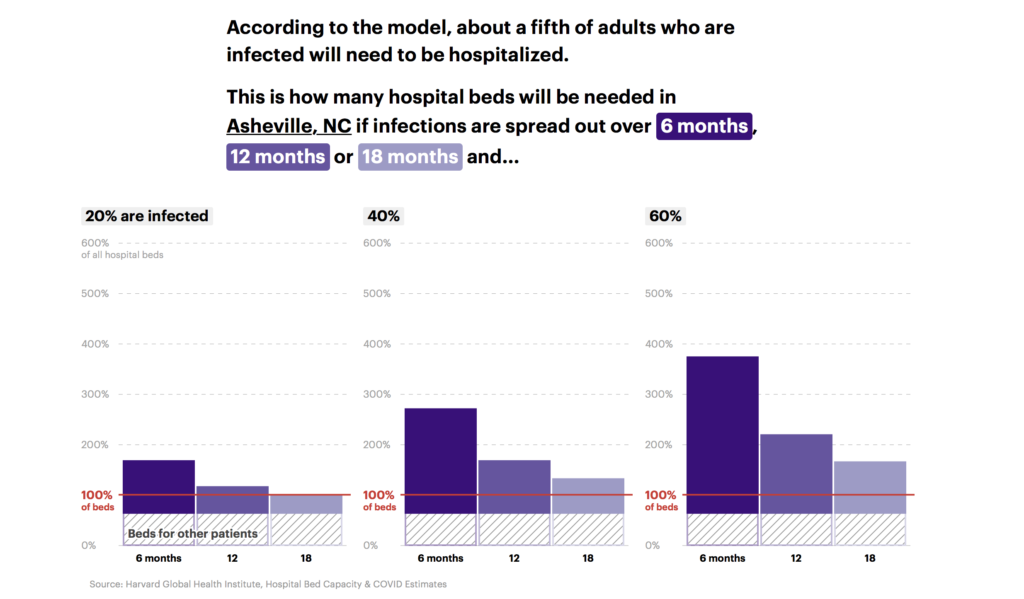
Source: Propublica.org
According to Duke, the Harris Regional Hospital in Jackson county is a 86-bed acute and specialty care facility serving a primary service area of the western North Carolina counties of Jackson, Swain, Graham, and Macon as well as parts of North Georgia.
Currently, according to NCDHHS Jackson County has three confirmed cases and two in Macon County; meanwhile, Swain and Graham counties have none. The CDC is calculating a second-wave to be even more devastating.
With the addition of a second wave, health care workers would be endangering themselves even more because some hospitals are lacking personal protective wear or PPE. Dr. Harkness is working in a hospital in Oregon where supplies are low resulting in physicians’ having to reuse masks.
“The needs are still PPE. That problem hasn’t been solved. We are still having to reuse masks. Hospital administration is trying to find ways to sanitize masks but these masks were never meant to be reused like that – the elastic starts to break down, which compromises the seal,” said Harkness.

Duke owned Harris Regional hospital serves the people of Jackson, Swain, Graham, and Macon as well as parts of North Georgia. Photo by WCJ archive.
As of right now, NCDHHS is reporting North Carolina to be extremely low in PPE such as gowns, face mask, coveralls and gloves. However, Harris Hospital in Jackson County says they have the necessary equipment for now.
“Our staff [has been] provided with appropriate PPE and we are not facing any supply issues at this moment,” Sara Crawford, Director of Marketing at Harris Hospital said in an email. Although they are not facing any issues at the moment, they are still accepting donations.
“As of right now, we are encouraging any and every one that feel led to contribute in whichever way they felt led. Donations have come in by way of meals to our staff while also supporting local business which is a win-win for everyone. We are accepting donations in the form of masks and gowns and although we are not asking for them, we are happy to receive them,” said Crawford.
In additional to PPE, testing for COVID-19 is limited.
“Testing right now is limited to people with symptoms or those hospitalized (this depends on where you live and what testing is available). If we could test everyone, we would be able to find out who the asymptomatic carriers are. But we don’t have the supplies for that yet,” said Dr. Harkness. “If we had more testing, we would have a better idea of the numbers. This would help people understand that they can be asymptomatic carriers; more people would understand staying at home and it will overall slow the spread.”
As of right now there is no permanent solution to the virus, however according to Harkness, “The ultimate final solution is a vaccine but expect it to be 1-2 years before we see that happen.”


